Month: June 2013
Analytical Method Validation
R One consequence of the robustness should be that a series of system suitability parameters (e.g. resolution test) is established to ensure that the validity of the analytical procedure is maintained whenever used.
Microbiology test of water ( IP,BP,USP)
Microbiology test of water ( IP,BP,USP)
Microbiological Test of Water is provided to determine compliance with the requirements given in individual monograph/specifications.
PRINCIPLE
Microbial testing of water includes the estimation of the number of viable aerobic bacteria present in a given quality of water.
MEDIA PREPARATION
Phosphate Buffer pH 7.2
Stock Solution
Dissolve 34 g of monobasic Potassium phosphate in about 500 mL of water contained in a 1 L volumetric flask. Adjust to pH 7.2 ± 0.1 by the addition of 4 % w/v aqueous solution of Sodium hydroxide (about 175 mL), add water to volume, and mix. Dispense, sterilize and store under refrigeration.
For use, dilute the Stock solution with water in the ratio of 1 to 800, and sterilize in an autoclave at 121 OC for about 15 min.
Nutrient Agar Medium
Beef Extract 10.0 g
Peptone 10.0 g
Sodium Chloride 5.0 g
Agar 12.0 g
Water 1000 mL
Dissolve with the aid of heat. Adjust to pH 8.0 to 8.4 with 5 M Sodium Hydroxide and boil for 10 min. Filter , adjust to pH 7.2 to 7.4 and sterilise by maintaining at 115 OC for 30 min.Soyabean Casein Digest agar
Pancreatic Digest of Casein 17.0 g
Papacy Digest of Soybean Meal 3.0 g
Sodium Chloride 5.0 g
Dibasic Potassium Phosphate 2.5 g
Dextrose (C6H12O6. H2O) 2.5 g
Agar 12.0 g
Distilled Water 1000 mL
Final pH after Sterilization 7.3 ± 0.2
Dissolve the solids in the water, warming slightly to effect solution. Cool to room temperature and add, if necessary, sufficient 0.1 N Sodium Hydroxide to give a final pH after Sterilization between 7.1 and 7.5. Filter, if necessary, to clarify, distribute into suitable containers and sterilize in an autoclave at 121 OC for about 15min.
MacConkey’s broth
Peptone 20.0 g
sodium Chloride 5.0 g
Sodium Taurocholate 5.0 g
Lactose 10.0 g
Bromocresol purple 10.0 mg
Water 1000 mL
Dissolve the Peptone, the Sodium Chloride taurocholate in the water with the aid of heat. Adjust to pH 8.0 and boil for 20 min. Cool, filter and adjust to pH 7.4. Add the Lactose and the indicator solution, mix and distribute in tubes containing inverted Durham’s tubes. Sterilize by maintaining at 121 OC for 20 min
For double strength medium, use double the quantity of ingredients in the same amount of water.
All the above media should be incubated for 24 h at 37 OC before use. Any contaminated media should be discarded.
Instead of preparing media, use dehydrated media of Hi media can be used. Re hydrate the required quantity as per instructions on the bottle label, dispense in required quantities and sterilize at 15 psi at 121 OC for 20 min.
PROCEDURE
A. WATER FOR INJECTION
Perform the Total microbial Count as follows :
Assemble the membrane filtration unit by keeping 0.45 µm filter membrane of the holder of the unit and moisten the membrane with distilled water. Autoclave the entire unit at
121 OC for 15 min. and allow to cool. Transfer 100 mL of water sample to the unit and filter it under aseptic conditions, by applying vacuum.
Transfer the membrane intended for enumeration of total bacterial count onto the surface of nutrient agar OR Soyabean casein digest agar and incubate at 37 OC + 2 °C for 3 days. Repeat the filtration process with 100 mL sample. Observe the plates for development of colonies and report the results as Colony forming units (CFU) per 100 mL sample.
B. PURIFIED WATER
1. TOTAL MICROBIAL
Perform the test for Total microbial count as follows :
1. Transfer aseptically 1 mL of the sample in each of two sterile Petri dishes.
2. Add to each dish approx. 20 mL of sterile nutrient agar / Soyabean casein digest agar previously cooled to about 45OC3. Cover the petridishes and mix the sample with the agar by rotating the dishes 3 times both in clockwise and anti-clockwise directions.
4. Allow the agar to solidify at room temperature.
5. Invert the petridishes and incubate them at 37 OC for 48 h.
6. After incubation, examine the plates for growth and count the number of colony forming units in each plate.
7. The average of both the readings is the total microbial count per mL.
C. POTABLE WATER
1. TOTAL MICROBIAL
Perform the Total microbial Count as follows .
1. Prepare 1/10 dilution of the water sample by transferring aseptically 10 mL of the sample to 90 mL sterile phosphate buffer pH 7.2
2. Transfer 1 mL from this to two sterile Petri dishes. Add sterile nutrient agar / Soyabean casein digest agar to them in the same manner as above and incubate at 37 OC for 3 days.
3. After incubation, note the number of colony forming units in each plate and calculate the average.
4. Multiply the average count by 10. The result is the Total microbial Count per ml
2. PATHOGENS
1. Perform the test for identification of Escherichia coli as per STP No. STP-046-00.
2. Perform the test for most probable number of coliforms as follows. Transfer aseptically 10 mL sample into each of five previously sterilized 10 mL double strength MacConkey’s broth tubes Similarly transfer 1 mL and 0.1 mL sample in 10 mL single strength MacConkey’s broth tube using 5 tubes for each sample quantity. Incubate all tubes at 37 OC for 48 h. and observe for gas production.
3 The number of positive findings of coliform group of organisms should be computed as the combination of positives and recorded in terms of most probable number (MPN) . The MPN for a variety of combinations isgiven in the Table I.
PRECAUTION
Keep adequate controls of Phosphate buffer pH 7.2, Nutrient agar and MacConkey Broth to confirm the validity of results.
POTABLE WATER
Observe the sample by physical examination in a 100 ml Nessler’s cylinder. The sample shall be clear.
2. ODOUR
Check the odour of the sample. Report for any unusual odour.
3. COLOUR
Principle :
Color is determined by visual comparison of the sample with known concentrations of colored solutions.
Sampling :
Collect representative samples in clean glassware. Make the colour determination within a reasonable period because biological or physical changes occurring in storage may affect color. With naturally colored waters these, changes invariably lead to poor results.
Apparatus : Nessler tubes, matched, 50 mL, of tall form.
Preparation of Standards :
1. Dissolve 1.246 g of Potassium Chloroplatinate [K2PtCl2], [eq. of 500 mg metallic Pt.] and 1.00 g of crystallized cobaltous chloride [CoCl2 6H2O], [eq. to 250 mg of metallic Co] in distilled water with 100 mL conc. HCl and dilute to 1000 ml with distilled water.This stock standard has a colour of 500 units.
2. Prepare standards having colors of 5, 10, 15, 20, 25, 30, 35, 40, 45, 50, 60, and 70, by diluting 0.5, 1.0, 1.5, 2.0, 2.5, 3.0, 4.0, 4.5, 5.0, 6.0, and 7.0 mL stock color standard with distilled water to 50 mL in Nessler Tubes.
Protect these colour standards against evaporation and contamination when not in use.
METHOD :
a. Estimation of Intact Sample
Observe sample color by filling a matched nessler’s tube to the 50 mL mark with sample and comparing it with standards. Look vertically downward through tubes toward a white or specular surface placed at such an angle that light is reflected upward through the columns of liquid. If the turbidity is present and has not been removed, report as ‘apparent color’. If the color exceeds 70 units, dilute sample with distilled water to known proportions until the color is within the range of the standards.
b. pH
Measure pH of each sample
Calculation (in case sample has been diluted)
Calculate color units by the following equations :
Color Units = [Estimated Color of diluted sample x 50 ] / mL sample taken for Dilution.
Reporting
Report color results in whole numbers and record as follows :
Color Units Record to Nearest
0 – 50 1
51 – 100 5
101 – 250 10
251 – 500 20
Report the sample pH.
4. pH
Instrument : The pH meter should be capable of reading with an accuracy of 0.05 pH Units.
Calibration with Standard Buffer solutions : Before sample pH measurement perform calibration of the instrument with pH 4.0 buffer and pH 9.0/9.2 buffer.
Sample measurement : Establish equilibrium between electrodes and sample by stirring sample to ensure homogenity ; Stir gently to minimize carbondioxide entrainment. Measure the sample pH at 25C.
Report pH value to the nearest 0.1 pH unit.
5. HARDNESS
Principle : Ethylenediaminetetracetic acid and its sodium salts [EDTA ] form a chelated soluble complex when added to a solution of certain metal cations. If a small amount of a dye such as Eriochrome BlackT or Calmaginte is added to an aqueous solution containing calcium and magnesium ions at a pH of 10.0 ± 0.1, the solution becomes wine red.
If EDTA is added as a titrant the calcium and magnesium will be complexed, and when all of the magnesium and calcium has been complexed the solution turns from wine red to blue, marking the end point of the titration. Magnesium ion must be present to yield a satisfactory end point.
Titration Precautions
Conduct titration’s at or near normal room temperature. The color change becomes impractically slow as the sample approaches freezing temperature. Indicator decomposition becomes a problem in hot water. Completion to the titration within 5 min. minimizes the tendency for CaCO3 , to precipitate.
Reagents :
Buffer Solution :
1. Dissolve 16.9 g Ammonium Chloride [(NH4Cl)], in 143 mL, conc. ammonium hydroxide [(NH4OH)]. Add 1.25 g magnesium salt of EDTA[commercially available ] and dilute to 250 mL with distilled water.
2. If the magnesium salt of EDTA is unavailable, dissolve 1.179 g disodium salt of ethylenediaminetetraacetic acid dihydrate (analytical reagent grade) and 780 mg magnesium sulfate [(MgSO4.7H2O)] or 644 mg magnesium chloride [(MgCL2.6H2O)] in 50 mL distilled water. Add this solution to 16.9 g NH4Cl and 143 mL of conc. NH4OH with mixing and dilute to 250 mL with distilled water. To attain the highest accuracy, adjust to exact equivalence through appropriate addition of a small amount of EDTA or MgSO4 or MgCl2.
Store Solution 1. and 2. in a plastic or borosilicate glass container for no longer than 1 month. Stopper tightly to prevent loss of ammonia [Nh3 ]
Indicator
Eriochrome Black T. : Sodium salt of 1-(1-hydroxy-2-naphthylazo)-5-nitro-2-naphthol-4-sulfonic acid; No.203 in the Color Index. Dissolve 0.5 g dye in 100 g 2,2’,2”-nitrilotriethanol (also called triethanolamine) or 2-methoxymethanol (also
called ethylene glycol mono methyl ether). Add 2 drops per 50 mL solution to be titrated. Adjust volume if necessary.
Standard EDTA Titrant, 0.01M : Weigh 3.723 g analytical reagent – grade disodium ethylenediaminetetraacetate dihydrate also called (ethylenedinitrilo) tetraacetic acid disodium salt (EDTA) , dissolve in distilled water, and dilute to 1000 mL , standardize against Standard Calcium Solution as described in method given below.
Standard Calcium Solution : Weigh 1.000 g anhydrous CaCO3 powder [primary standard or special reagent low in heavy metals, alkalis, and magnesium] into a 500 mL erlemeyer flask. Place a funnel in the flask neck and add, a little a time, 1+1 HCl until all CaCO3 has dissoved. Add 200 mL distilled water and boil for few minutes to expel CO2 . Cool, add a few drops of methyl red indicator, and adjust to the intermediate orange color by adding 3N NH4OH or 1+1HCl, as required. Transfer by quantitatively and dilute to 1000 mL with distilled water: 1 mL = 1.00 mg CaCO3.
Method
Titration of Sample
Select a sample volume that requires less than 15 mL EDTA titrant and complete titration within 5 minutes measured from time of buffer addition.
Dilute 25.0 sample to about 50 mL with distilled water in a porcelain casserole or other suitable vessel. Add 1 to 2 mL buffer solution. Usually 1 mL will be sufficient to give a pH of 10.0 to 10.1. The absence of a sharp end-point color change in the titration usually means that an inhibitor must be added at this point or that the indicator has deteriorated.
Add 1 to 2 drops indicator solution or an appropriate amount of dry-powder indicator formulation. Add Standard EDTA titrant slowly, with continuous stirring, until the last reddish tinge disappears. Add the last few drops at 3- to 5-s intervals.
At the end point the solution normally is blue. Daylight or a daylight fluorescent lamp is recommended highly because ordinary incandescent lights tend to product a reddish tinge in the blue at the end point.
Calculation :
Hardness (EDTA) as mg CaCO3 / L =
[mL titration for sample x mg CaCO3 , equivalent to 1.00 m L EDTA titrant]
mL sample.
6. CHLORIDE
Principle
In a neutral or slightly alkaline solution, potassium chromate can indicate the end point of the silver nitrate titration of chloride. Silver chloride is precipitated quantitatively before red silver chromate is formed.
Apparatus :
– Conical flask, 250 mL
– Burette, 50 mL.
Reagents :
Potassium Chromate Indicator Solution : Dissolve 50 g K2CrO4 in a little distilled water. Add AgNO3 solution until a definite red precipitate is formed. Let stand 12 h, filter, and dilute to 1 L with distilled water.
Standard Silver Nitrate Titrant, 0.0141 M (0.0141N): Dissolve 2.395 g AgNO3 in distilled water and dilute t 1000 mL. Standardize against NaCl by the procedure of “Titration” described below. 1.00 mL = 500 µg of Cl-.
Special Reagents for Removal of Interference :
Aluminium Hydroxide Suspension : Dissolve 125 g aluminium potassium sulfate or aluminum ammonium sulfate, AlK(SO4)2.2H2O or AlNH4(SO4)2.12H2O, in 1 L distilled water. Warm to 60o C and add 55 mL conc. ammonium hydroxide (NH4OH) slowly with stirring. Let stand about 1h, transfer to a large bottle, and wash precipitate by successive additions, with thorough mixing and decanting with distilled water, until free from chloride . When freshly prepared, the suspension occupies a volume of approximately 1L.
Phenolphthalein Indicator Solution
Sodium Hydroxide, NaOH, 1N :
Sulfuric acid, H2SO4, 1N
Hydrogen Peroxide, H2O2, 30% :
Method :
Sample Preparation : Use a 100 ml sample or a suitable portion diluted to 100 mL. If the sample is highly colored, add 3 mL Al(OH)3 suspension, mix, let settle, and filter. If sulfide, sulfite, or thiosulfate is present, add 1 mL H2O2 and stir for 1 min.
Titration :Directly titrate samples in the pH range 7 to 10. Adjust sample pH to 10 with H2SO4 or NaOH if it is not in this range. For adjustment, preferably use a pH meter with a non-chloride-type reference electrode. (If only a clhloride-type electrode is available, determine amount of acid or alkali needed for adjustment discard this sample portion.
Treat a separate portion with required acid or alkali and continue analysis.) Add 1.0 mL indicator solution. Titrate with standard AgNO3 titrant to a pinkish yellow end point. Be consistent in end-point recognition.
Standardize AgNO3 titrant and establish reagent blank value by the titration method outlined above. A blank of 0.2 to 0.3 mL is usual.
Calculation :
mg Cl- / L =
(mL, titration for sample – mL titration for blank) x Normality of AgNO3 x 35.450
mL of sample
7. TOTAL DISSOLVED SOLIDS Dried at 105oC
Principle :
A well-mixed sample is filtered through a standard glass fiber filter, and the filtrate is evaporated to dryness in a weighed dish and dried to constant weight at 105oC. The increase in dish weight represents the total dissolved solids.
Apparatus :
– Filtration apparatus : One of the following, suitable for the filter
disk selected.
– Membrane filter funnel.
– Gooch crucible, 25 mL to 40 mL capacity, with Gooch crucible
adapter.
– Filtration apparatus with reservoir and coarse (40- to 60- µm)
– fritted disk as filter support.
– Suction flask, of sufficient capacity for sample size selected.
– Drying oven, for operation at 105 ± 2oC.
Method :
Preparation of glass-fiber filter disk : Insert disk with wrinkled side up into filtration apparatus. Apply vacuum and wash disk with three successive 20 mL
volumes of reagent-grade water. Continue suction to remove all traces of water. Discard washings.
Preparation of Evaporating Dish : If volatile solids are to be measured, ignite cleaned evaporating dish at 550o for 1 h. in a muffle furnace. If only total dissolved solids are to be measured, heat clean dish to 105 ± 2oC for 1 h in an oven . store in desiccator until needed. Weigh immediately before use.
Selection of Filter and Sample Sizes : Choose sample volume to yield between 10 and 200 mg dried residue. If more than 10 minutes are required to complete filtration, increase filter size or decrease sample volume. When very low total suspended solids are encountered (less than 10 mg/L), less dried residue may be collected; compensate by using a high-sensitivity balance (0.002 mg)
Sample Analysis :
Stir sample with a magnetic stirrer and pipette a measured volume onto a glass-fiber filter with applied vacuum. Wash with three successive 1 mL volumes of reagent-grade water, allowing complete drainage between washings, and continue suction for about 3 minutes after filtration is complete. Transfer total filtrate (with washings) to a weighed evaporating dish and evaporate to dryness on a steam bath or in a drying oven.
If necessary, add successive portions to the same dish after evaporation. Dry evaporated sample for at least 1 h. in an oven at 105 ± 2oC, cool in a desiccator to balance temperature, and weigh. Repeat drying cycle of drying, cooling, desiccating, and weighing until a constant weight is obtained or until weight change is less than 4% of previous weight or 0.5 mg, whichever is less. Duplicate determinations should agree within 5% of their average.
Calculation :
mg, total dissolved solids / L (ppm)=
{ [(Weight of dried residue + dish, mg) – Weight of dish, mg] x 1000 }
/sample volume mL
8. MICROBIAL LIMITS
Determine total plate count and absence of pathogens as per the current version
PROCEDURE FOR DECONTAMINATION OF D. M. WATER PLANT
1.0 AIM
To lay down a standard operating procedure for Decontamination of D.M. Water plant.
2.0 SCOPE
Maintenance Department
3.0 AREA OF OPERATION
Service floor.
4.0 RESPONSIBILITY
Operator/Maintenance Supervisor concerned.
5.0 ACCOUNTABILITY
Maintenance Incharge.
6.0 PROCEDURE
NOTE: Decontamination of D.M. Water plant is done as per recommendation of Q. C. department or once in a month; after regeneration of D.M. Water Plant.
6.1 Decontamination of Mixed Bed Unit
a) Mix 40 ml of formaldehyde solution with 200 ltr of D.M Water.
b) Inject this solution into mixed bed unit (MBU) by dipping tube attached to ejector E-2 into the formaldehyde solution and by opening valve 18, 20 & 22.
c) After completion of formalin injection close the valve 18, 20 & 22.
6.2 Decontamination of anionic exchanger
a) Mix 40 ml of formaldehyde solution with 200 ltr. D. M. Water.
b) Deep the tube attached to ejector into formaldehyde solution.
c) Open valve 4, 5, 6, 7 and adjsut valve 4 to maintain the flow.
d) After completion of injection close the valce 4, 5, 6 & 7
6.3 Decontamination of Cationic exchanger
a) Mix 40 ml of formaldehyde solution with 200 ltr. D.M. Water.
b) Deep the tube attached to ejector into formaldehyde solution.
c) Open valve 1, 2 & 3 and adjust the valve 2 to maintain the flow.
d) After completion of injection close the valce 1, 2, & 3.
6.4 Rinsing of columns
a) Next day start the D.M. Water plant (Ref. SOP-ME- ) and drain the water.
b) Give the sample of D. M. Water to Q.C.
c) After getting OK from Q. C. collect the D. M. Water into D. M. Water collection tank.
7.0 REVIEW DATE
After 2 years or when procedure is changed
DO YOU KNOW IF (OR WHEN) A PRODUCT IS CONSIDERED MEDICINAL IN THE UK?
What is a medicine? What is a cosmetic, a food, a food supplement, a device? What happened to unlicensed herbal remedies? Do you have a product which you think might be considered a borderline substance, somewhere between a number of the above classes?
What is a disease?
You will find helpful information about the UK’s position on these subjects in the revised MHRA Guidance Note No. 8
The document is not a complete or definitive statement of the law and it is not intended as a substitute for legal or other professional advice but you might be surprised about what you learn.
DO YOU KNOW IF (OR WHEN) A PRODUCT IS CONSIDERED MEDICINAL IN THE UK?
What is a medicine? What is a cosmetic, a food, a food supplement, a device? What happened to unlicensed herbal remedies? Do you have a product which you think might be considered a borderline substance, somewhere between a number of the above classes?
What is a disease?
You will find helpful information about the UK’s position on these subjects in the revised MHRA Guidance Note No. 8
The document is not a complete or definitive statement of the law and it is not intended as a substitute for legal or other professional advice but you might be surprised about what you learn.
DO YOU KNOW IF (OR WHEN) A PRODUCT IS CONSIDERED MEDICINAL IN THE UK?
What is a medicine? What is a cosmetic, a food, a food supplement, a device? What happened to unlicensed herbal remedies? Do you have a product which you think might be considered a borderline substance, somewhere between a number of the above classes?
What is a disease?
You will find helpful information about the UK’s position on these subjects in the revised MHRA Guidance Note No. 8
The document is not a complete or definitive statement of the law and it is not intended as a substitute for legal or other professional advice but you might be surprised about what you learn.
Designating API starting materials acceptably in a chemical synthesis
Making the correct designations of ‘active substance starting materials’ in a chemical synthesis can be very difficult but is extremely important to your company. There is a subjective element to overcome and only a limited set of rules to help you with the decisions. These will be discussed and some examples considered in our comprehensive CTD Module 3 course in London on 2 – 3 July 2013.
The impact of the designations on GMP compliance with regard to development costs and to the time taken to gain regulatory approvals of Marketing Authorisation applications can be huge, so increasing your understanding of the many issues is more than sensible! Please hurry to book if you want to secure a place. Bookings close soon.
EMA releases draft policy for clinical trial data transparency
June 25 2013 | By Márcio Barra

The European Medicines Agency (EMA) has just released for consultation a draft policy on access and transparency of clinical-trial data. This draft details three levels of access according to the type of data, alongside rules for publication and use.
View original post 368 more words
Supervision of Chinese-Made Drug Substances by Philippe André
Why source drug substances from China?
Large markets, economies of scale and cheaper labor;An industrial ecosystem supplying raw materials and equipment;Developed infrastructure and industry friendly policies;About 5,000 manufacturers;
Thousands of chemists and students across China looking for novel synthesis routes for generic drug substances and intermediates.
read all at
http://www.allfordrugs.com/2013/06/21/supervision-of-chinese-made-drug-substances-by-philippe-andre/
Genotoxic Impurities In Pharmaceuticals
Decisions to approve, prescribe and consume medicines involve risk/benefit assessments by regulatory agencies, health care professionals and consumers. For serious or life threatening conditions, drugs with higher risks for adverse effects or for serious adverse effects are sometimes acceptable. For example, some life-saving cancer chemotherapies are known human carcinogens. However, if one is suffering from a life threatening tumor, a 5% risk of a secondary, treatment-related tumor is generally considered acceptable. Arguably, the same is not true for impurities found in drug substances and drug products; impurities convey only risk with no associated benefit. Drug impurities might be viewed as “pollutants” in the pharmaceutical world. Much like pollutants in the environment, few people believe that they can be entirely eliminated. The challenge for regulatory agencies is to promulgate standards that assure that unavoidable drug impurities impart no or acceptable levels of risk.
read all at
http://www.pharmainfo.net/reviews/genotoxic-impurities-pharmaceuticals
Tecfidera’s impressive launch hit by supply and reiumbursement problems
June 20 2013 | By Márcio Barra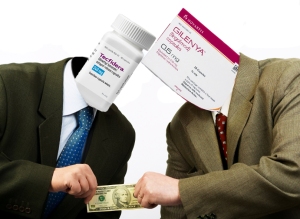
Tecfidera, Biogen’s idec of first-line oral treatment for people with relapsing forms of Multiple Sclerosis approved back in March in the US and EU, is having a very impressive start, selling so well that it’s expected to break the blockbuster barrier by next year according to the The Wall Street Journal. But the demand is such among patients, doctors and pharmacies that supply hasn’t been able to fully satisfy the demand. Supply chain and manufacturing snags also interfered with distribution, said Biogen’s CEO George Scangos.
View original post 252 more words
Guideline on the European Drug Master File Procedure updated
Guideline on the European Drug Master File Procedure updated
http://www.gmp-compliance.org/ecanl_619_0_news_3750_7935,S-RGL_n.html
The “Guideline on Active Substance Master File Procedure” which was developed by EMA’s Quality Woring Party, describes the procedure that can be used to document an API’s quality for a regulatory authority. This guideline was already revised several times since it was initially issued in 2006. The last update was published in October 2012. This 3rd revision was updated again now to “support the Working Group on Active Substance Master File Procedures in their initiatives to improve the ASMF procedure across the European Regulatory Network” as mentioned in the remarks on page 2 of the Guideline.
The Guideline comprises updates mainly referring to its Annexes:
- Annex 1: In part 3.2.S.2.1 of the ASMF all sites where manufacturings steps (e.g. the manufacturing of intermediates, quality controls, in-process controls, milling and sterilisation processes) take place have to be indicated.
- Annex 2: With this Letter of Access the API manufacturer (ASMF Holder) grants the authority insight into the ASMF’s restricted part. According to the respective passage which was included in the letter template, the API manufacturer agrees that the authority exchanges the ASMF evaluation reports with the EDQM’s certification department.
- Annex 3: This “Submission Letter and Administrative Details for documents relating to an ASMF” has to be submitted together with the ASMF as part of a new marketing authorisation application or a variation. The updated template of this letter comprises much more detailed requirements. For instance, the active substance (where applicable) has to be specified regarding its salt form, water content and grade.
- Annex 4: Withdrawal of Access Letter. With this letter the ASMF Holder can withdraw the authorisation for the authority to use the ASMF (restricted part). The reasons for this can be the termination of API manufacture or the replacement of the ASMF procedure by the CEP procedure (CEP = Certificate of Suitability). This Annex is new.
- The Annexes 5, 6 and 7 (previously Annexes 4 and 5) were modified only slightly. The glossary (Annex 7) includes references to the respective VICH GL39-Guideline which is based on ICH Q6A.
The Guideline text itself was adapted according to the updated Annexes.
Please see the “Guideline on Active Substance Master File Procedure”; CHMP/QWP/227/02 Rev 3/Corr” for more detailed information.


